Polypharmacy for dietitians. Dr Natali Jokanovic & Dr Amanda Cross
 Chloe Risaglu, APD
Chloe Risaglu, APD
The most common definition of polypharmacy is the ‘regular use of five or more medications.’ In Australia, polypharmacy occurs in 36% of people aged over 70 (a similar figure to New Zealand), a number that increases in hospital inpatients (75%), and aged care residents (82%). Some of the most common medications contributing to polypharmacy include PPIs and medications to manage cholesterol blood pressure, diabetes, anxiety, and depression.
Aside from patient burden and compliance issues, polypharmacy poses other risks. It increases the danger of an adverse drug event, and the chance of medications interacting with any other medications, supplements, medical conditions, or food. Additionally, individuals taking 10 or more medications (hyper polypharmacy) are at a higher risk of malnutrition.
Medications which may contribute to nutritional deficiencies include:
- PPI’s – can cause low magnesium, calcium, and vitamin B12 if taken for a prolonged period
- Metformin – can cause low folic acid and vitamin B12
- Statins – can contribute to low levels of CoQ10
Medications which may interact with food include:
- Warfarin – vitamin K
- Statins – grapefruit
- Metronidazole - alcohol
Due to our detailed client assessments, dietitians are well positioned to identify polypharmacy in patients, and suggest if a comprehensive medication review would be beneficial. A pharmacist medication review may result in a simplified medication regime, reduction in medication dose, or utilise combination products if possible.
Red flags which suggest that a medication review from a pharmacist may be appropriate include:
- Polypharmacy – taking five or more medications
- Being unable to describe the medications they are taking, and how frequently they are taking them
- There is a prescribing cascade- a medication side effect is treated with another medication
- Non-adherence to medications (eg. if a patient tells you they take a medication ‘sometimes’ or ‘when they remember’)
- Risk of nutrient deficiencies from their medication
- Being overwhelmed with their medication regime
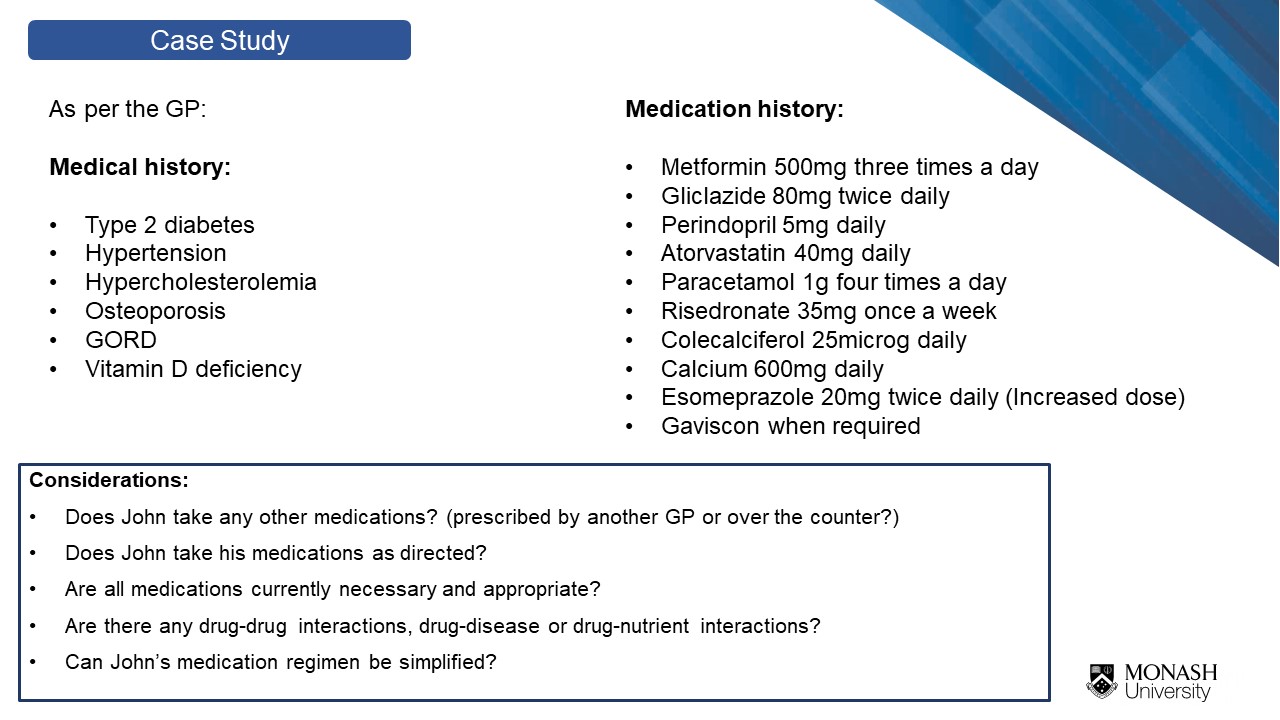
In this presentation, Natali and Amanda discuss the process the pharmacist goes through when conducting a medication review, including how they may manage and simplify a patient’s medications. Additionally, they highlight a case study commonly seen in practice: demonstrating how a patient may present to us, key factors that indicate they may need a medication review, and how a pharmacist would approach managing their medications.
Dr Amanda Cross BPharm (Hons) GradCert (Pharm Prac), PhD is a research fellow in dementia at the Centre of Medicine Use and Safety at Monash University. She also works as a pharmacist in the community, and as a home medication review pharmacist. Amanda completed her PhD in 2019 at Monash University, focusing on optimising medication use and medication management, and has 13 articles published in scientific journals. Amanda is an active member of the Pharmaceutical Society of Australia.
Dr Natali Jokanovic BPharm (Hons) GradCert (Pharm Prac), PhD is a hospital pharmacist and researcher based at Department of Infectious Diseases at the Alfred Hospital and Monash University. In 2019 she completed her PhD at Medicine Use and Safety, Monash University, focusing on understanding and addressing polypharmacy in residential aged care.
To access the presentation and assessment quiz, click here