Oral allergy syndrome. Presented by Ingrid Roche, APD
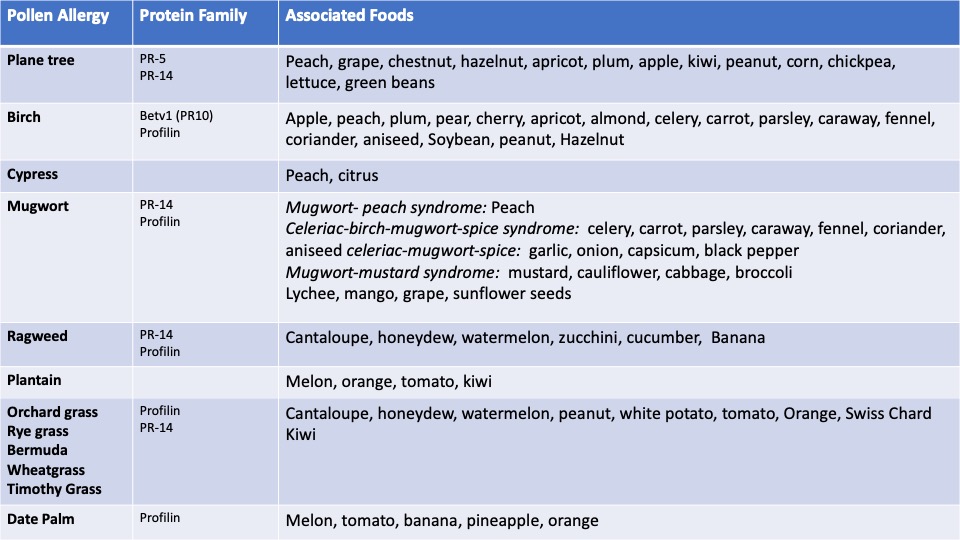
Oral allergy syndrome (the preferred term is pollen-food allergy syndrome) is an allergy to fruits and vegetables that occurs in people who have a pollen allergy. It is estimated to occur in 7-10% of the population. Typically there is itching and/or mild swelling of the mouth and throat after eating raw fruits, vegetables or nuts. The symptoms result from contact urticaria in the oropharynx from pollen related proteins in these foods. People with pollen-food allergy syndrome can go on to develop systemic allergic reactions including anaphylaxis.
Signs and symptoms of oral allergy syndrome are similar to food chemical intolerance, so it is important for us to be able to distinguish between them to ensure we provide appropriate treatment and management.
Ingrid uses a clinical case to help explain:
1. How a diagnosis of pollen-food allergy syndrome is arrived:
- Oral symptoms of itching and swelling and the timing of symptoms indicate more of an immediate food allergy rather than a delayed intolerance type symptom profile.
- A history of hay fever points towards pollen-food allergy syndrome.
Ultimately diagnosis is made by an allergist who will see:
- Evidence of sensitisation to plant food in question – using fresh foods and commercial extracts
- Evidence of allergic sensitisation to pollen
- A correlation between the plant and pollens the patient is sensitised to
2. Medical management:
- Dietary Avoidance of the food
- Antihistamine (not routinely recommended)
- Adrenaline
- Pollen Immunotherapy
- SLIT (food)
- Anti IgE therapy (omaluzimab)
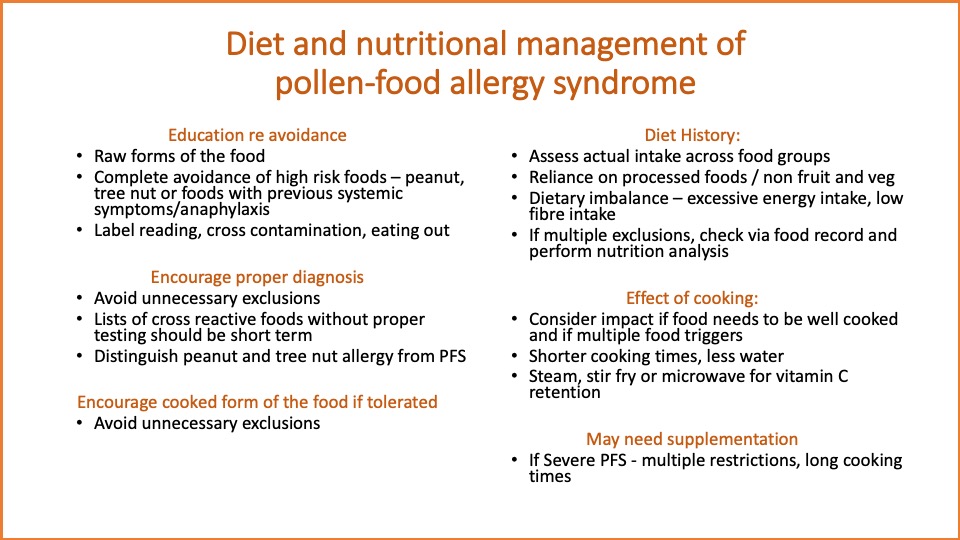
3. Dietary and nutritional management:
- Education re avoidance
- Ensure proper diagnosis
- Encourage eating a cooked form of the food if tolerated
- Diet history- consider supplementation
Ingrid Roche has been an Accredited Practising Dietitian since 1995 and has developed her expertise in food allergy over the past 11 years working at the Perth Children’s Hospital (formerly Princess Margaret Hospital) in the field of allergy and immunology. She also has a private practice in Perth. Ingrid was chair of the Dietitian’s Committee of the Australasian Society for Clinical Immunology and Allergy (ASCIA) from 2012 – 2018, during which time the ASCIA e-training dietitians was developed; as well as the ASCIA-CAL advanced learning course in food allergy in partnership with Dietitians Australia. She remains an active member of ASCIA and Allergy & Anaphylaxis Australia and is currently project co-lead on the food service project of the National Allergy Strategy. Ingrid is committed to providing and improving training in food allergy for health and other professionals, as well as improving the quality life for consumers and families living with food allergy.
To register for the presentation and associated documents including the assessment quiz click here