Nutrition in people with advanced dementia- Part 1: Nutritional assessment by Isabelle Goodwin, APD
 Anthea Talliopoulos, APD
Anthea Talliopoulos, APD
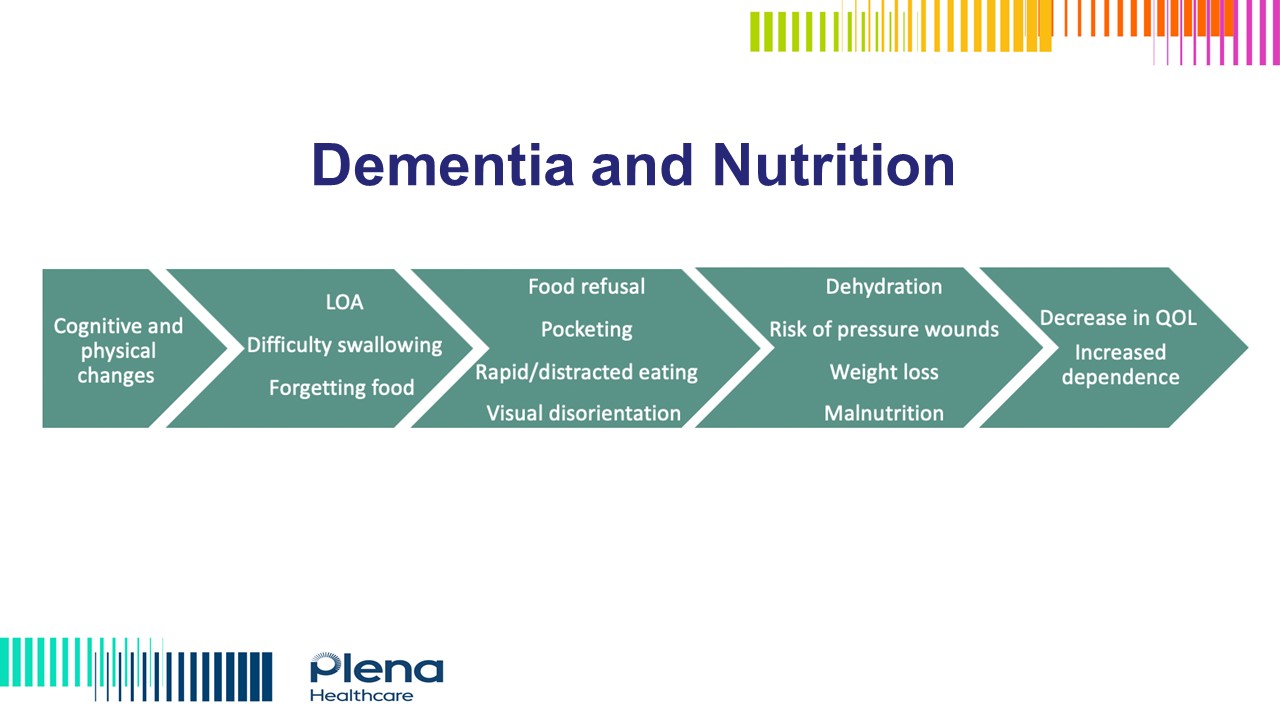
Dementia is a growing public health issue, continuing to increase in prevalence, being the second leading cause of death in Australia and the leading cause of death in women. With 68% of aged care residents having dementia, many elderly Australians are either personally effected by dementia themselves or know someone who they are in close contact with who has dementia. Dementia can have a significant impact on nutrition such as through effecting appetite, reducing fine motor skills, increasing energy and protein requirements as a result of wandering, and overall increasing dependence and the risk of malnutrition.
In understanding the nutritional impact of advanced dementia, Accredited Practising Dietitian Isabelle Goodwin talks through a clinical scenario of an aged-care resident, discussing all key aspects of a patient-centred nutritional assessment and intervention through an anthropometric, biochemical, clinical and dietary format. In obtaining anthropometric data, the appropriateness of physical assessments (such as the SGA) should be considered as obtaining consent may be difficult and may also impact the mood and overall comfort of the patient. In requesting biochemistry, routine biochemical screening is not standard practice and should only be considered if this is practical and clinically indicated, such as in the case of suspected deficiencies or refeeding syndrome.
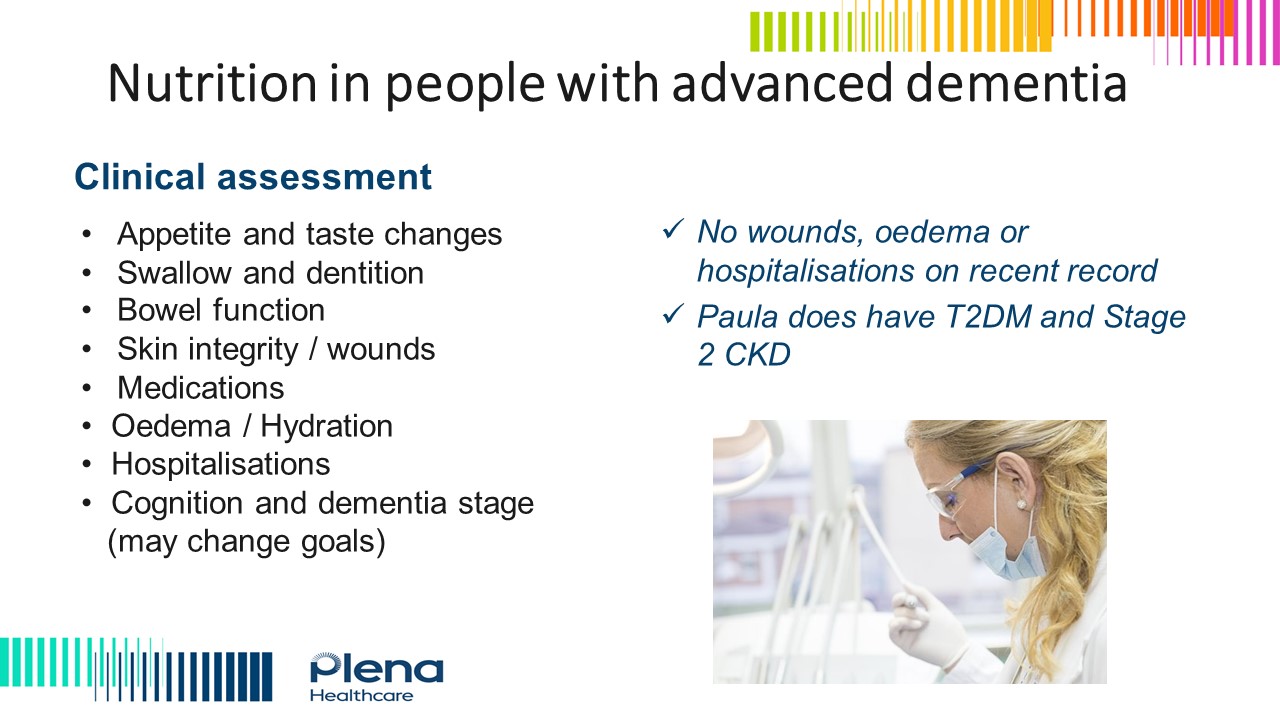
Important clinical information should be assessed, such as appetite, dentition, bowel function, medications, oedema, and the stage of dementia. In addressing dietary practices, the Montessori Method in dementia should also be considered as this may increase the capacity of patient to self-feed. Further to this, dietary and mood behaviours such as the time of day that mood and appetite are best should ideally be taken into account, as well as any strategies which can help to increase meal acceptance.
As a whole, the nutritional management of dementia is complex, and it is crucial that patient-centred care is provided to overcome any nutritional barriers and prevent malnutrition.
Summary:
- Dementia is a growing public health issue, continuing to increase in prevalence, being the second leading cause of death in Australia and the leading cause of death in women and effecting 68% of aged care residents.
- Dementia can have a significant impact on nutrition such as through effecting appetite, reducing fine motor skills, increasing energy and protein requirements as a result of wandering, and overall increasing dependence and the risk of malnutrition.
- Completing a thorough nutritional assessment is crucial, considering the comfort and behaviour of the patient, any clinical barriers, and practical strategies to increase meal acceptance.
- The nutritional management of dementia patients is complex and should be individualised and interpreted in collaboration with all clinical data to best support patients living with this condition.
Isabelle Goodwin, APD currently works in the Tasmanian community as a residential aged care dietitian and also in private practice. With a strong interest in mental health and associated conditions, Isabelle completed further research into nutrition in dementia care in 2020 and published this research in 2022. Isabelle is also a credentialed eating disorder clinician (CEDC) and supports undergraduate health students at The University of Tasmania through tutoring and marking.
To register for the presentation and associated documents including the assessment quiz click here