Enteral nutrition case studies, Sarah Marfurt, APD
 Anthea Talliopoulos, APD
Anthea Talliopoulos, APD
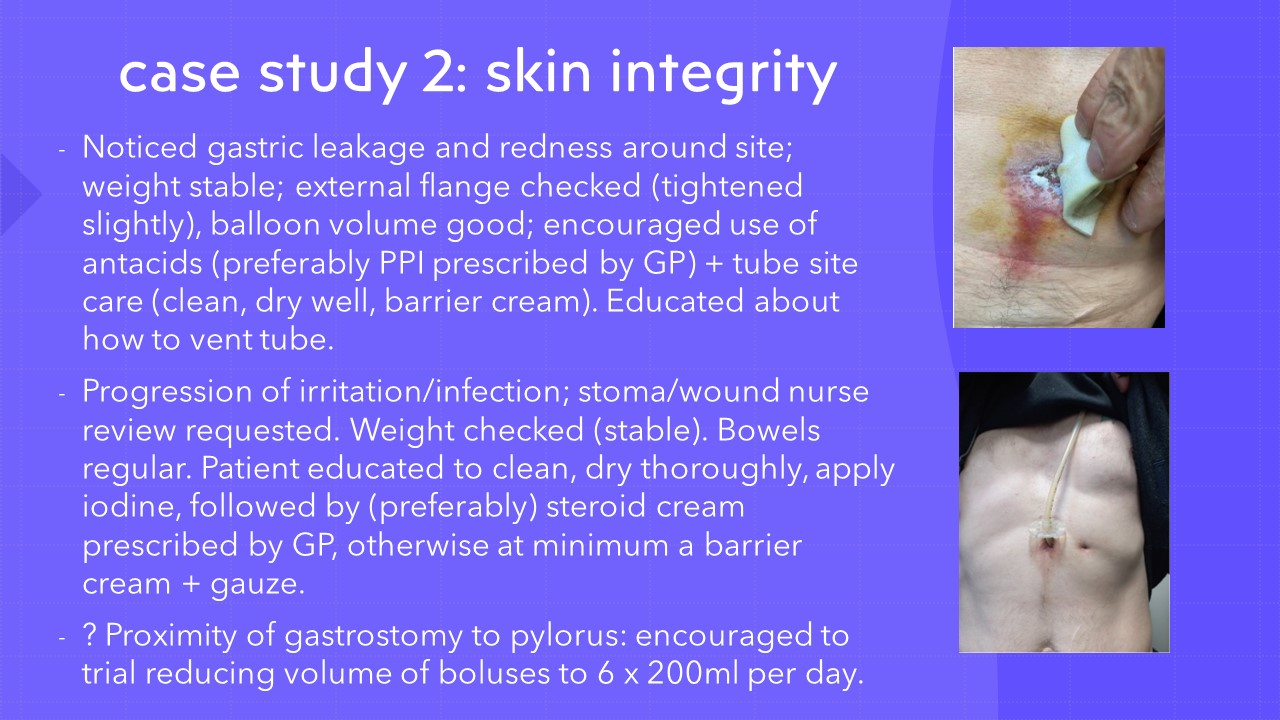
With different feeding modes, potential complications, ethical considerations, and often multiple comorbidities to consider, enteral nutrition can be a confusing space to navigate. However, advocating for an enteral feed and supporting patients in the long-term management of their nutrition can have a significant impact on their nutritional status. While an ideal feed rate may be determined, feeding and tube complications, such as through home enteral nutrition, can inevitably result, posing a challenge moving forwards.
In this practical presentation, Accredited Practising Dietitian Sarah Marfurt shares her knowledge and expertise on enteral nutrition through multiple case studies, in each of which the management, feeding regimen and clinical indications differ. She explains the importance of liaising with General Practitioners in the case of home enteral nutrition to ensure medical follow-up is provided within the out-patient setting. This can be critical in terms of altering prescribed medications such as proton pump inhibitors, prokinetics, antiemetics and laxatives, all of which may assist in meeting the feeding regimen. Such medications can be useful in reducing reflux, nausea, early satiety, and altered bowel habits, assisting in implementing the dietetic treatment plan.
Sarah also discusses the importance of working with and educating the family and/ or carers (such as in the case of supporting NDIS participants) in successfully implementing home enteral nutrition. Ethical considerations such as the prognosis of patients is also discussed, as indicated in the ASPEN clinical guidelines, in ensuring that quality of life is prioritised.
Overall, it is critical that we work holistically in considering home enteral nutrition pathways in clinical practice, in support patients to optimise their nutritional status and best manage their clinical symptoms.
Summary:
- Multiple considerations must be taken into account in the implementation of home enteral nutrition, including the home environment, supports, medical follow-up, feeding regimen and ethics.
- The management of clinical symptoms is key- such as nausea, vomiting, reflux and altered bowel habits, all of which may disrupt the feeding regimen, including the chosen feed formula.
- Key clinical guidelines such as from the Agency for Clinical Innovation, APSEN, EPSEN and the British Dietetic Association should also be considered in implementing enteral nutrition.
- It is critical that advice provided is tailored to the needs of the patient in optimising their nutritional status and in ensuring that the feeding regimen is appropriate.
Sarah Marfurt, APD has a special interest in gastrointestinal nutrition and home enteral feeding. Sarah provides individualised care for her patients, empowering them to take their health into their own hands. The clinical scenarios she will use in this presentation are from her work at La Trobe Regional Hospital in Gippsland, Victoria. They will illustrate the range of skills and flexible approach working in a regional area requires. Last month, Sarah took a role at the Alfred Hospital in Melbourne.
To register for the presentation and associated documents including the assessment quiz click here