Continuous glucose monitoring by Dr Camel Smart, PhD, APD
 Anthea Talliopoulos, APD
Anthea Talliopoulos, APD
As health professionals, it is crucial that we are informed of the devices and options for glucose monitoring in assisting individuals living with type 1 diabetes as this will impact on their treatment options and specific dietary management. One of these options includes continuous glucose monitoring (CGM), which provides excellent data regarding trends and information about changes in glucose levels in a convenient and relatively non-invasive way. CGM are small wearable devices which can be scanned when desired to measure the glucose level of interstitial fluid and can be used with or without the automation of insulin delivery through a pump. It is important to note that while CGM provides valuable information, is does not measure blood glucose levels specifically, and while interstitial fluid is usually within 2mmol of the blood glucose levels, this can vary. CGM does, however, identify useful information on post-prandial increases in blood glucose levels, which is a key influencing factor on HbA1C.
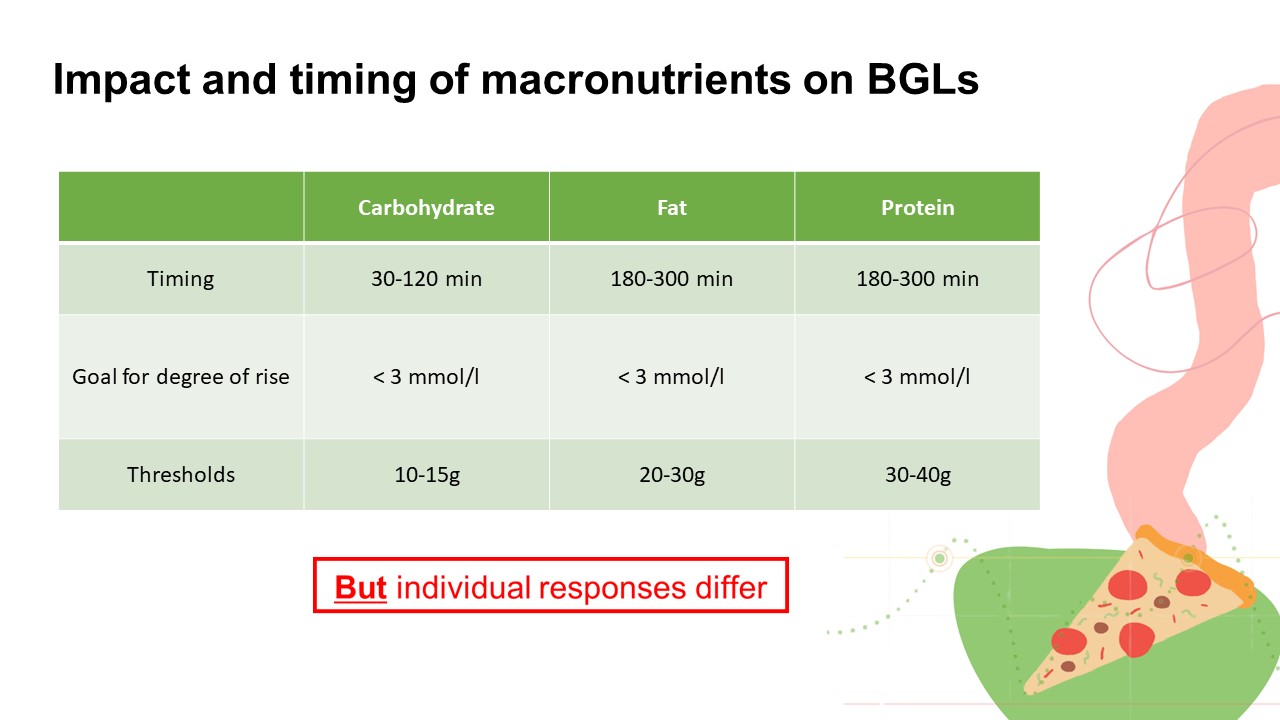
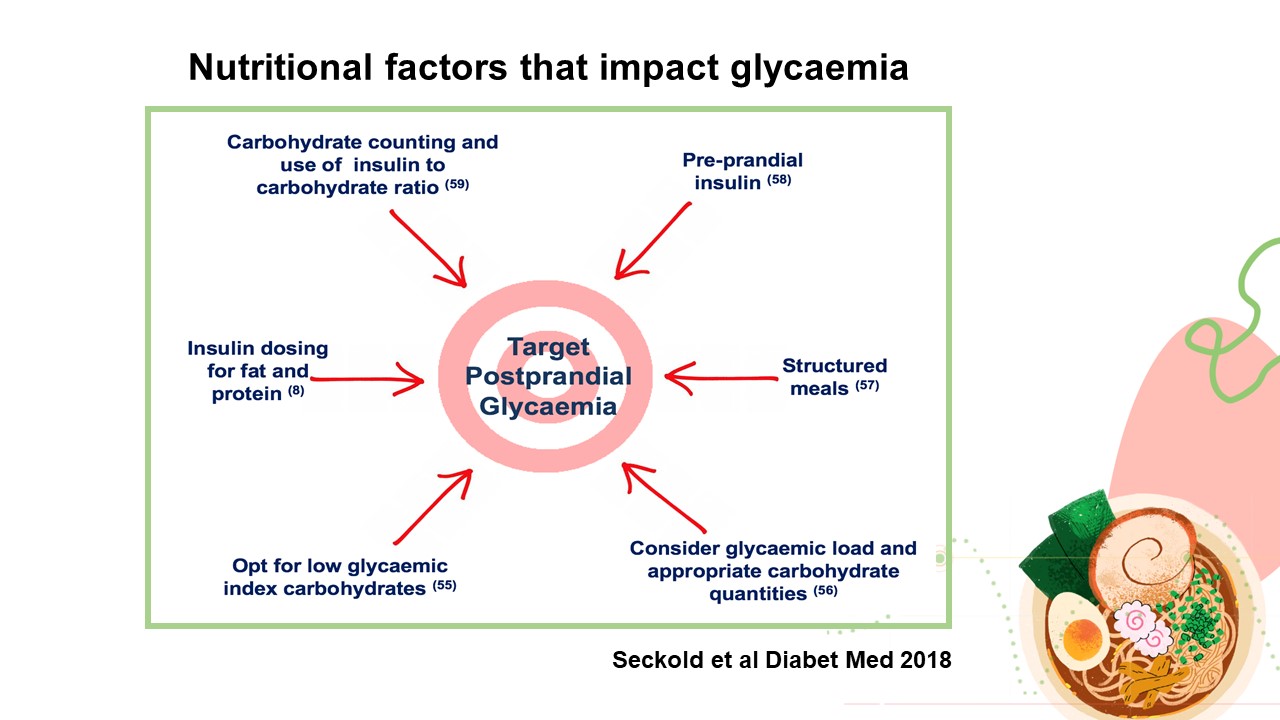
In this informative and in-depth presentation, Accredited Practising Dietitian Dr Camel Smart shares her knowledge and expertise on the benefits, practicality, and interpretation of continuous glucose monitoring, with specific examples, in relation to food intake and dietary behaviours. She provides a background on the CGM devices available, glucose targets, and the impact and timing of different macronutrients on glucose levels, emphasising the importance of establishing a regular eating routine.
As type 1 diabetes is a specialised area, it is essential that dietitians seeking to work in this space find mentoring or supervision so that safe, high-quality care is provided.
Summary:
- Continuous Glucose Monitoring (CGM) measures interstitial glucose levels, providing valuable data on trends and post prandial glucose levels (a key influencing factor on time in range and HbA1C).
- With CGM becoming more readily available and subsidised for healthcare card holders or individuals <21 years of age, it is crucial that we as dietitians know when to recommend it, assist individuals in how to interpret it, and how to provide tailored dietary recommendations to optimise glycaemic control.
- Given the specifics of type 1 diabetes, advancements in technology and the importance of tailored care, continuing education, professional supervision or mentoring is highly recommended in dietitians who are seeking to move into this space.
Dr Carmel Smart is an international authority on nutrition and type 1 diabetes who works as a Senior Specialist Diabetes Dietitian at the John Hunter Children’s Hospital, Newcastle, NSW, Australia. She is an active clinician researcher and has published widely on the impact of food and strategies to optimise blood glucose levels after eating. Carmel holds posts on the Australian Dietetics Council and the Australasian Paediatric Endocrine Group and is a member of the Living Evidence clinical guidelines writing group for the management of Type 1 Diabetes. In 2019 Carmel was a recipient of the Michelle Beets award for outstanding achievement in advancement of children’s health in type 1 diabetes and the Hunter Children’s Medical Foundation Outstanding Researcher.
To register for the presentation and associated documents including the assessment quiz click here