Pursuing a Career as an Allergy Specialist Dietitian
 Amanda Jackson, APD and Marianne Tomlin, APD
Amanda Jackson, APD and Marianne Tomlin, APD
Are you interested in becoming an allergy specialist Dietitian? With the incidence of food allergy on the rise, the need for expert advice in this area is increasing. Melbourne based allergy specialist dietitians and members of the ASCIA Dietetic Group Amanda Jackson and Marianne Tomlin have put together a check list to help you make your next career move.
What makes a good allergy specialist Dietitian?
Allergy is a multidisciplinary speciality, so you need to be a good team player with an investigative mind and attention to detail. The ability to take an excellent detailed history is fundamental to determining which food(s) (if any) the individual is reacting to.
Patients and carers are often highly anxious and need practical ways to eliminate allergens from the diet whilst also meeting their nutritional needs specific to their age and gender. Understanding the food labelling laws and having an interest in allergen free recipe development and cooking is useful. Having willing friends, family, or colleagues to sample your “free from” recipes is always a bonus!
What type of clients or conditions do you see?
In Paediatrics we tend to see children whose parents have been advised to avoid sometimes a vast range of allergens from their child’s diet either as a preventative measure (due to a sibling allergy) or where the child has shown symptoms that they may be suffering from a possible food allergy (such as severe eczema, passing mucosy stools or urticaria). Sometimes the number of foods excluded is quite large and the child (and breastfeeding mother) are left with nutritionally inadequate diets. We spend a lot of time unpicking the true adverse food reaction(s) and optimising their nutritional status either through reintroduction of foods where appropriate or recommended nutrient dense safe alternative foods. Children may have a combination of a severe life-threatening food allergy, a delayed food allergy/intolerance or Food Protein-Induced Enterocolitis Syndrome. We have also been able to eliminate all of these diagnoses in some children and referred them to the Gastroenterology team where they have then been correctly managed for Eosinophilic Oesophagitis or a functional gut disorder.
In the Adult setting, we see patients with lifelong food allergies (not outgrown in childhood) and adult-onset food allergies that can develop at any age. A few conditions we see more commonly amongst adult patients include Pollen Food Allergy Syndrome (also known as Oral Allergy Syndrome) and Food Dependent Exercise Induced Anaphylaxis. There can also be cross over with patients with suspected food allergies that go on to be diagnosed with a food intolerance and gastrointestinal conditions such as Eosinophilic Oesophagitis and IBS that may require further dietary manipulation.
What are some of the nutritional challenges?
The potential for harm is high in food allergy. Without access to appropriate dietetic support and suitable food replacements nutritional deficiencies can develop including protein, vitamin B12, calcium and iron to name a few. Restrictive diets can also lead to poor growth in children, unintentional weight loss and malnutrition in adults and development of eating disorders.
Here is a table summarising some of the main nutrients which are at risk with dietary exclusion.
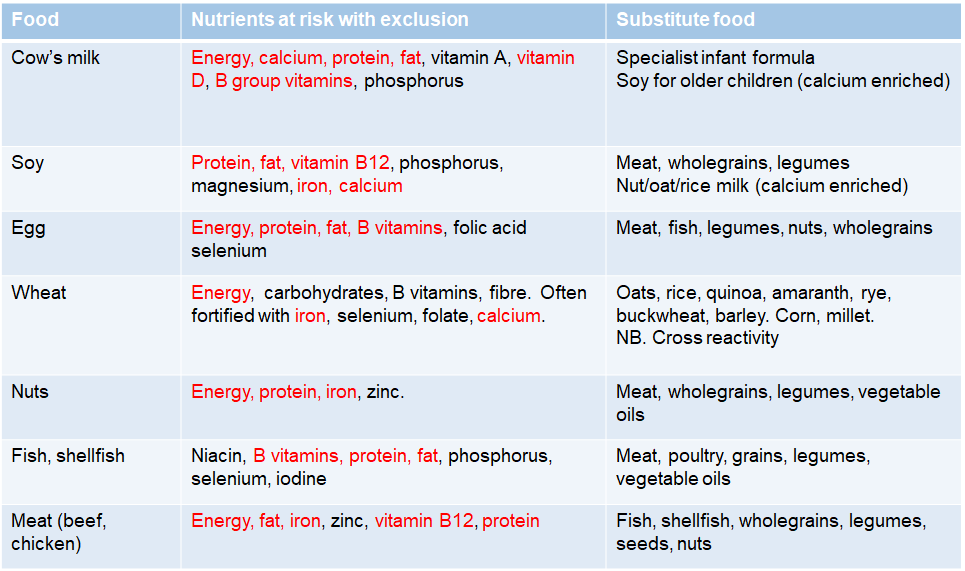
Table 1. Identifying Nutrients at risk with Exclusion Diets
The lack of psychosocial support is also challenging and can impact on individual’s adherence to health and nutrition advice with increased rates of anxiety, depression and overall reduced quality of life identified in food allergy sufferers.
What are the differences seen working in the world of allergy rather than other areas of dietetics?
The dietitian is a highly respected and valued member of the allergy team and component of successful allergy service. They are often privileged to be involved in the patient and family’s journey across the lifespan from initial diagnosis through to long term management.
Where can you learn more and keep up to date?
There are lots of fabulous resources available for you to learn more and opportunities for ongoing practice development including:
ASCIA : vast range of latest patient resources, health professional e-learning modules, clinical guidelines and the annual scientific conference which includes a “dietitians day” i.e. a full day of dietitian specific professional development
National Allergy Strategy
Allergy & Anaphylaxis Australia
Food Standards of Australia and New Zealand
Dietitians Australia
Place journal alerts with key words so you are notified with the latest allergy publications
Where could I look for work?
If you are working in the community or clinical setting, raise your interest in obtaining experience in allergy at your next supervision meeting. There may be potential shadowing opportunities or ability to attend training events or a course to further your knowledge. Once you have some background allergy knowledge you could also contact your local allergy centres to inquire about potential training roles or opportunities for regular shadowing.
It is also a good idea to learn what allergy free products are in the supermarket and online, so you start to become familiar with available food alternatives. It is always worth having a try so you can give some real-life feedback to your patients as they always want to know “which tastes best?!”
Good luck with your next steps!
Amanda Jackson, Accredited Practising Dietitian
Amanda Jackson is an Accredited Practising Dietitian with expertise in management of adult food allergies, intolerances, gastrointestinal diseases, kidney disease and immune disorders. She has over 13 years’ experience and first developed her interest in food allergy working in The Alfred Hospital’s Allergy, Asthma and Immunology Department. Amanda then moved to Royal Melbourne Hospital and whilst working for the Clinical Nutrition Department successfully established the allergy and immunology nutrition service. Amanda is passionate about improving the health and wellbeing of adults with food allergies and immune disorders and continues to work at RMH today as the Senior Dietitian for the Clinical Immunology and Allergy Department. She also has a private clinic at Melbourne Allergy Asthma and Immunology Consultants.
Her roles see her involved in resource development, teaching and training to both the dietetic and broader allergy community - from consumers through to the multidisciplinary healthcare team. She is an active member of Dietitians Australia, Allergy & Anaphylaxis Australia and the Australasian Society of Clinical Immunology and Allergy (ASCIA) – including participation within the Dietitians Committee and the National Immunodeficiency Strategy as the sole allied health representative.
Marianne Tomlin, Accredited Practising Dietitian
Marianne Tomlin is a Melbourne based Accredited Practising Dietitian, with extensive experience in childhood food allergies, both in the UK and Australia. Marianne has a particular interest in feeding difficulties in children with food allergies and has recently established a new allergy feeding clinic at Monash Children’s Hospital. She also is part of the allergy team at The Royal Children’s Hospital and runs two private clinics via Kids Nutrition Clinic and Offspring Health.